Pesticide exposure remains a serious and common health risk among agricultural workers in the United States. Clinicians often miss pesticide exposure because the symptoms at times are nonspecific; a strong medical history can greatly assist in uncovering potential exposures.
“Workers exposed to pesticides, they typically present with very vague symptoms, systemic systems as well, so you might get workers who present with a little bit of nausea or vomiting, or gastrointestinal symptoms, or you might get workers with respiratory symptoms,” noted Brett Shannon, MD, PhD, occupational and environmental medicine specialist, in a recent three-part webinar series on pesticides, presented in English and Spanish by Migrant Clinicians Network. Data that he pulled from Illinois state pesticide reporting pointed to dermatological, asymptomatic, and neurological symptoms as the top signs and symptoms, expanding the range of symptoms a clinician must look for. “I think this is why we miss a lot of cases… Sometimes the clinical picture is not so clear, that a worker is being exposed to pesticides,” he explained. “If a worker presents with very vague or very generalized symptoms, it’s really important to ask about exposure to pesticides as part of your clinical history and consider it as a potential exposure because of the kind of symptoms we’re seeing.”
Determining Exposure Scenario
Taking a thorough occupational history is an important way to understand the circumstances surrounding a pesticide exposure. Identifying the exposure scenarios including the source of the exposure helps clinicians in their diagnosis. Also, considerations like the nature of the task or job, use of personal protective equipment, and type of space such as an enclosed space like a greenhouse are relevant when assessing the exposure scenario. The route of exposure, determining if the exposure was dermal, inhaled, ocular, or ingested, is also important.
Four Areas of Questioning
Dr. Shannon generally focuses on four areas of questions when triaging a patient exposed to pesticides. First, he asks about general health concerns the patient may have, such as any major health problems, their range of symptoms – whether they are localized or systemic -- and whether the patient could be pregnant. Second, he asks questions about the specific incident and what they were doing at the time of exposure. Third, he inquires about their job, the nature of their role, and the tasks they do each day. He asks his patients to give him a rundown of what a typical day looks like. Lastly, he wants to know if they have been getting any kind of treatment, if they’ve seen another provider for this issue, or if they have been self-treating.
Organophosphates, Pyrethroids, and Rodenticides
To best interpret the medical history, clinicians need a basic understanding of the acute health effects of each class of commonly used pesticide. Organophosphates cause acute symptoms like nausea, dizziness, breathing difficulties, and, in severe cases, nerve damage, paralysis, and death. Pyrethroids are synthetic versions of natural pyrethrins found in chrysanthemum flowers. They are generally less toxic but can still cause skin irritation and respiratory problems and can affect the nervous system. Long-term exposure to either pesticide has been linked to potential neurological and developmental issues. Rodenticides, used to kill rodents, are harmful to humans if swallowed, inhaled, or touched. They can cause symptoms like nausea, dizziness, internal bleeding, and organ damage. Some rodenticides are anticoagulants and can cause serious bleeding. Others can affect the nervous system or kidneys.
Once an exposure is confirmed, Dr. Shannon underscores the value of determining which specific pesticide was used – and reviewing the information on that pesticide’s label. Data to collect from the acutely exposed patient includes contaminated clothing, a urine sample, and other samples as needed.
Effects of the Exposure
In treating exposed patients, the effects and subsequent treatment will depend on the type of pesticide, the dose, routes of exposure, distribution, metabolism, elimination, and individual sensitivity. Age -- especially if the patient is a child – gender, the possibility of pregnancy, health status, genetics, and concurrent exposures such as use of pesticides at home all impact how an individual will respond to the exposure.
Acute pesticide exposure and long-term exposure may each result in chronic health effects. During the webinar, Dr. Shannon reviewed some of the evolving findings regarding chronic pesticide exposure including among children who are vulnerable. The research has shown neurodevelopmental delays from exposure to the fetus in pregnant women and to children at young ages. Pesticide exposure is also associated with attention deficit hyperactive disorder and autism spectrum disorder. For adults, Dr. Shannon shared that there is a diagnosis called chronic organophosphate neuropsychiatric disorder that involves mood instability, suicidal ideation, and cognitive impairment. Agricultural workers exposed to pesticides may face a wide range of long-term health issues; for example, research suggests associations between pesticide exposure and Parkinson’s disease, certain kinds of cancers, and endocrine disruption.
Taking a Holistic Approach
Dr. Shannon encourages clinicians to think about exposures in the larger context, including the mental health of the patient. “Too many times…we focus on the pathology or the red flags for these chemical exposures including pesticides. We treat the pathology instead of treating the patient holistically,” he said. “It’s very important to consider that any exposure to pesticide or any other work hazard is a very traumatic experience for many workers. It’s something that could potentially kill them, it’s something that’s very scary for them. And you have to consider this and consider examining their mental health during and after the incident.” He emphasized the importance of looking at additional factors including job status, access to insurance, ongoing exposures, and fear of retaliation after reporting of the exposure. “I think [asking these additional questions] is almost just as important as the pesticide exposure itself,” Dr. Shannon said. “We can treat the pesticide exposure, but the trauma can stay for many many years.”
Pesticide Clinical Tools and Resources
|
Acute Pesticide Exposure Clinical Guidelines MCN's Pesticide Clinical Guidelines and Pesticide Exposure Assessment Form assists in the recognition and management of acute pesticide exposures in primary care settings. |
|
|
Cholinesterase Testing Protocols and Algorithm These clinical tools provide a concise and simple format for clinicians to use as guides in managing care for patients working with Class I and Class II organophosphates (OP) or OP and N-methyl-carbamates. |
|
|
Recognition and Management of Pesticide Poisonings EPA’s Recognition and Management of Pesticide Poisonings, 6th Edition, is an essential guide for health care providers on pesticide toxicology, diagnosis, and treatment. Includes a comprehensive index of signs and symptoms and important resources. https://www.epa.gov/pesticide-worker-safety/recognition-and-management-pesticide-poisonings |
|
|
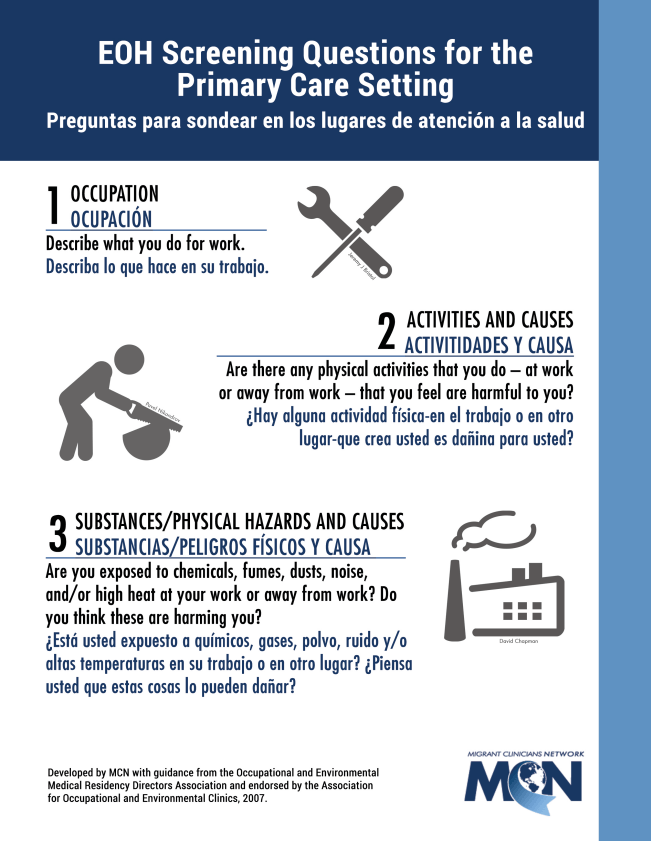
Environmental and Occupational Health Screening Questions for Primary Care Three concise and effective environmental/occupational health screening questions for the primary care provider. English and Spanish. |
Resource
- MCN's three-part webinar series, "How to Prevent Pesticide Poisoning in Farmworkers" is available to watch at: https://www.migrantclinician.org/webinar/ diagnosis-and-management-pesticide- related-illness-how-prevent-pesticide-poisoning